The
thoracic cage is formed by the vertebral column behind, the ribs and intercostal
spaces on either side and the sternum and costal cartilages in front. Above, it
communicates through the ‘thoracic inlet’ with the root (BASE) of the neck; below, it is separated from the abdominal
cavity by the diaphragm (Fig. 1).
The diaphragm is the dome-shaped septum (DIVING WALL OR
PARTITION) dividing the thoracic from the abdominal cavity. It comprises two
portions: a peripheral (OF OR RELATING TO THE SURFACE OR OUTER
PART OF A BODY OR ORGAN) muscular part
which arises from the margins of the thoracic outlet and a centrally
placed aponeurosis (A SHEETLIKE FIBROUS MEMBRANE RESEMBLING A
FLATTENED TENDON THAT SERVES AS A FASCIA TO BIND MUSCULES TOGETHER OR TO
CONNECT MUSCLE TO BONE)(Fig. 10).
The muscular fibres are arranged in three parts.
1◊◊Avertebral part from the crura (AN
ELEONGATED PART OF AN ANATOMICAL STRUCTURE) and from the arcuate
ligaments (REFERS TO AN ARC-SHAPED LIGAMENT).
The right crus (SEE CURA) arises from
the front of the bodies of the upper three lumbar vertebrae (ONE
OF THE FIVE HUMAN VERTEBRAE GROUPS) and intervertebral discs (A
CARTLIGOUS DISC SERVING AS A CUSHION BETWEEN ALL OF THE VERTEBRAE IN THE SPINAL
COLUMN EXCLUDING THE FIST TWO) the left crus is only attached
to the first two vertebrae.
The arcuate ligaments are a series of fibrous arches,
the medial (IN THE MEDIAN PLANE OF THE BODY OR
THE MIDLINE F AN ORGAN) being a thickening of the fascia covering psoas
major (A LARGE MUSCLE THAT RUNS FROM THE LUMBAR SPINE THROUGH THE
GROIN ON EITHER SIDE) and the lateral(SIDE) of
fascia overlying quadratus lumborum (A MUSCLE IN THE BACK
WHICH ATTACHES TO THE TOP OF THE PELVIS AND THE SPINE IN THE UPPER LUMBAR
AREA). The fibrous medial borders of the two crura form a median
arcuate ligament over the front of the aorta.
2◊◊Acostal part is attached to the inner
aspect of the lower six ribs and costal
cartilages.
3◊◊Asternal portion consists of two small
slips from the deep surface of the
Xiphisternum. The central tendon, into which the muscular fibres are
inserted, is trefoil
in shape and is partially fused with the under-surface of the
pericardium.
The diaphragm receives its entire motor supply from the phrenic nerve
(C3, 4, 5) whose long course from the neck follows the embryological migration
of the muscle of the diaphragm from the cervical region (see below). Injury or
operative division of this nerve results in paralysis and elevation of the
corresponding half of the diaphragm.
Radiographically (IN X-RAYS),
paralysis of the diaphragm is recognized by its elevation and paradoxical (SELF-CONTRADICTORY)
movement; instead of descending on inspiration it is forced upwards by pressure
from the abdominal viscera (INTERNAL ORGANS).
The sensory nerve fibres from the central part of the diaphragm also run
in the phrenic nerve, hence irritation of the diaphragmatic pleura (PART
OF THE PARIETAL PLEURA)(in pleurisy) or of the peritoneum on the undersurface
of the diaphragm. Subphrenic collections of pus or blood produces referred pain
in the corresponding cutaneous (AFFECTING OR RELATED TO THE
SKIN) area, the shoulder-tip. The peripheral part of the diaphragm, including
the crura, receives sensory fibres from the lower intercostal nerves.
Openings in the diaphragm
The three main openings in the diaphragm (Figs 10, 11) are:
1◊◊the aortic (at the level of T12)
which transmits the abdominal aorta, the thoracic duct and often the azygos
vein;
2◊◊the oesophageal (T10) which is
situated between the muscular fibres of the right crus of the diaphragm and
transmits, in addition to the oesophagus, branches of the left gastric artery
and vein and the two vagi (EACH OF THE TENTH PAIR OF CRANIAL
NERVES, SUPPLYING THE HEART, LUNGS, UPPER DIGESTIVE TRACT, AND OTHER ORGANS OF
THE CHEST AND ABDOMEN);
3◊the opening for the inferior vena cava (T8)
which is placed in the central tendon and also transmits the right phrenic
nerve.
In addition to these structures, the greater and lesser splanchnic
nerves pierce the crura and the sympathetic chain passes behind the diaphragm
deep to the medial arcuate ligament.
The development of the diaphragm and the anatomy of diaphragmatic herniae (A
CONDITION IN WHICH PART OF AN ORGAN IS DISPLACED AND PROTRUDES THROUGH THE WALL
OF THE CAVITY CONTAINING IT).
The development of the diaphragm and the anatomy of diaphragmatic herniae
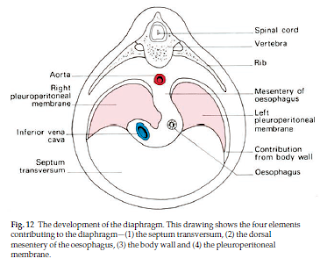
The diaphragm is formed (Fig. 12) by fusion in the embryo of:
1◊◊the septum transversum (forming the central
tendon);
2◊◊the dorsal oesophageal mesentery;
3◊◊a peripheral rim derived from the body wall;
4◊◊the pleuroperitoneal membranes,
which close the fetal communication between the pleural and peritoneal
cavities.
The septum transversum is the mesoderm (THE MIDDLE LAYER OF AN EMBRYO IN EARLY
DEVELOPMENT, BETWEEN THE ENDODERM AND ECTODERM) which, in early
development, lies in front of the head end of the embryo. With the folding off
of the head, this mesodermal mass is carried ventrally (NEAR
THE ABDOMEN) and caudally (TOWARD THE POSTERIOR END OF THE BODY), to lie in its definitive position at the anterior (TOWARD
THE FRONT OF THE BODY) part of the diaphragm.
During this migration, the cervical myotomes (PART OF
EMBRYONIC VERTEBRAE) and nerves contribute muscle and nerve supply respectively,
thus accounting for the long course of the phrenic nerve (C3, 4 and 5) from the
neck to the diaphragm. With such a complex embryological story, one may be
surprised to know that congenital abnormalities of the diaphragm are unusual.
However, a number of defects may occur, giving rise to a variety of
congenital
herniae through the diaphragm. These may be:
1◊◊through the foramen of Morgagni (UNCOMMON
DIAPHRAGMATIC HERNIAE); anteriorly between the xiphoid and costal origins;
2◊◊through the foramen of Bochdalek—the
pleuroperitoneal canal—lying posteriorly;
3◊◊through a deficiency of the whole central tendon
(occasionally such a hernia may be traumatic in origin);
4◊◊through a congenitally large oesophageal hiatus (PAUSE,
BREAK). Far more common are the acquired hiatus herniae
(subdivided into sliding and rolling herniae). These are found in patients
usually of middle age where weakening and widening of the oesophageal hiatus
has occurred (Fig. 13).
In the sliding hernia the upper stomach and lower
oesophagus slide upwards into the chest through the lax hiatus when the patient
lies down or bends over; the competence of the cardia (THE
UPPER OPENING OF THE STOMACH, WHERE THE ESOPHAGUS ENTERS) is often disturbed
and peptic juice can therefore regurgitate into the gullet. This may be
followed by oesophagitis with consequent heartburn, bleeding and, eventually,
stricture formation.
In the rolling hernia (which is far less common) the
cardia remains in its normal position and the cardio-oesophageal junction is
intact, but the fundus (THE UPPER PART OF THE STOMACH, WHICH
FORMS A BULGE HIGHER THAN THE OPENING OF THE ESOPHAGUS) of the stomach rolls up
through the hiatus in front of the oesophagus, hence the alternative term of
para-oesophageal hernia. In such a case there may be epigastric
discomfort, flatulence and even dysphagia, but no regurgitation
because the cardiac mechanism is undisturbed.
The movements of respiration
During inspiration the movements of the chest wall and diaphragm result
in an increase in all diameters of the thorax. This, in turn, brings about an
increase in the negative intrapleural pressure and an expansion of the lung
tissue. Conversely, in expiration the relaxation of the respiratory muscles and
the elastic recoil of the lung reduce the thoracic capacity and force air out
of the lungs.
In quiet inspiration the first rib remains relatively
fixed, but contraction of the external and internal intercostals elevates and,
at the same time, everts the succeeding ribs. In the case of the 2nd–7th ribs
this principally increases the anteroposterior diameter of the thorax (by the
forward thrust of the sternum), like a pump handle.
The corresponding movement of the lower ribs raises the costal margin
and leads mainly to an increase in the transverse diameter of the thorax, like
a bucket handle. The depth of the thorax is increased by the contraction of the
diaphragm which draws down its central tendon. Normal quiet expiration,
brought about by elastic recoil of the elevated ribs, is aided by the tone of
the abdominal musculature which, acting through the contained viscera, forces
the diaphragm upwards.
In deep and in forced inspiration additional muscles attached to the
chest wall are called into play (e.g. scalenus anterior,
sternocleidomastoid,
serratus anterior and pectoralis major) to increase further the capacity
of
the thorax. Similarly, in deep expiration, forced contraction of the
abdominal
muscles aids the normal expulsive factors described above.




No comments:
Post a Comment